How can we manage pain using Yoga Therapy?
Acknowledgement – School of Yoga is deeply grateful to late Dr. V. Sivaraman for his collaboration of pain management using Yoga therapy.
Introduction to pain.
Pain is caused by an unpleasant stimulus. Consequently, it becomes a stressor which destabilises homeostasis. As a result, the body’s adoptive response mechanism initiates physiological responses to meet the threat. However, prolonged exposure to the lifesaving chemicals triggered by the response can result in harmful side effects.
Importantly, though pain is noxious and unpleasant, it is a powerful protective force. Pain sends a signal that the body needs protection and healing. But, if correction does not occur, or the pain persists, the pain may become chronic. Therefore, pain must be contained or relieved.
What are the effects of pain?
-
- Cardiovascular – increased heart rate, blood pressure, need for oxygen, potential water retention resulting in fluid overload.
- Respiratory – increased respiratory rate, shallow breathing resulting in increased risk of infection.
- Immune/ endocrine system – activation of the HPA (Hypothalamus/ Pituitary/ Adrenal) axis, increased cortisol and glucose production.
- Gastro-intestinal & kidneys – reduced motility and emptying (reduced peristalsis) or constipation and increased urge to urinate.
- Musculo-skeletal – bunching of muscles at the point of pain, shaking and shivering
- Nerves / psychological – depression, anxiety and poor concentration.
What is the role of the Sympathetic Nervous System (SNS) in pain?
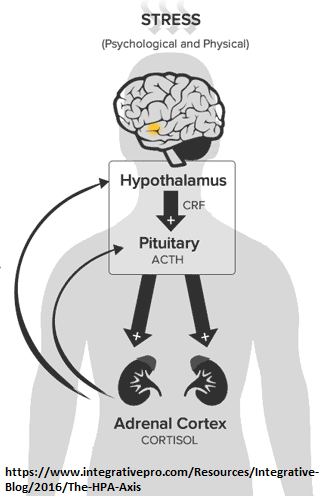
The body’s response to pain is centered around the Sympathetic Nervous System (SNS). The SNS reaction to pain is similar to fear and invokes a “fight or flight” response. To start with, the amygdala is activated by the pain. Immediately, the amygdala drives the hypothalamus to produce corticotrophin-releasing hormone (CRH). Next, this stimulus is transmitted to the pituitary gland which activates the Sympathetic Nervous System to release the production of adrenocorticotrophin (ACTH). Finally, the SNS also stimulates the adrenal medulla to release noradrenaline, serotonin and endogenous opioids into the dorsal horn.
As a result, there is stimulation of the heart and lungs, resulting in increased heart rate, blood pressure and respiratory rate. Consequently, there is increased blood supply to the musculo-skeletal system. This also results in reduced supply to the digestive system resulting in reduced secretion of digestive enzymes and peristaltic action. This results in a reduced ability to digest food, nausea, vomiting and constipation.
The side effects of the these drugs are,
- Brain: Altered balance between limbic and frontal cortex control of micturition.
- Heart: Increased heart rate, contractility and speed of conduction resulting in increased heart rate and blood pressure.
- Blood flow: Reduced blood flow to skin. Also, there is dilation of blood vessels going to the muscles.
- Kidneys: Reduced blood flow to kidneys (Increased glomuerular filteration rate). Also, these is increased production of antidiuretic hormone (leading to water retention), increased production of renin and increased retention of sodium.
 Stomach: Reduced peristalsis leading to reduced digestion, nausea and constipation.
Stomach: Reduced peristalsis leading to reduced digestion, nausea and constipation.- Liver / pancreas: Increased metabolic rate – conversion of glycogen to glucose (to provide energy for “fight or flight” response), reduced insulin production (increased blood glucose).
- Musculo-skeletal system: Shaking and shivering. Teeth chattering can occur.
The level of cortisol in the blood provides a feedback mechanism to the hypothalamus, thereby preventing over-release.
Under normal circumstances, this mechanism is effective in reducing pain and preventing inflammatory response from getting out of control. However, long term stress and pain results in continuous production of cortisol which leads to resistance in the glucocorticoid receptors and impairs feedback to the hypothalamus. Consequently, cortisol slowly loses its ability to keep inflammation under control. Also, higher levels of inflammatory mediators can lead to depression, anxiety and sleeplessness.
What are the implications of chronic pain?
Pain induces a variety of interrelated changes in several body systems. During the critical phase, these interventions are lifesaving and helpful in containing and relieving pain. However, over time, these responses result in potentially harmful side-effects, especially in patients whose reserves are already low.
Normally, a person in extreme pain will display elevated heart rate, blood pressure and respiratory rate. Also, they may shiver; have fever, goose bumps and pale skin. However, in case of chronic pain, these symptoms might not be exhibited unless the patient’s condition deteriorates. Hence, such indicators are often misleading and unreliable. So, it is important that the patient is constantly assessed for pain through various validated tools. This will help in effective pain management.
Very acute and chronic pain is called fibromyalgia.
Efect of pain on the immune system
All damage to tissue triggers the immune system which is based on the production of adrenocorticotrophin (ACTH). This results in blood vessel dilation and permeability to facilitate translocation of immune cells to the point of injury. Eventually, the quickened permeation also results in reduced oxygen content in the blood stream and this can have long term impact on the overall physiological health of the person.
Effect of pain on mood

Pain triggers an emotional response orchestrated by the various regions of the cortex – the amygdala, hypothalamus, brain stem and modulatory system.
Often, a high level of pain induces strong emotions such as fear or intense anxiety. Consequently, this leads to high state of arousal which can result in reduced sensitivity to pain. Similarly, a low or moderate state of arousal could lead to a lowered sensitivity to pain, making pain more easily felt.
Therefore, assessment of mood is very important for the right treatment and support to be given.
School of Yoga explains hormones which allow the body to manage pain
-
Cortisol
Cortisol is a steroid hormone that regulates many processes within the body, from metabolism to control of salt and water balance which affects blood pressure. Also, it plays an important role in the body’s response to pain. Pain induces the Sympathetic Nervous System to release the production of adrenocorticotrophin (ACTH). Unfortunately, chronic pain can lead to continuously elevated levels of cortisol and adrenal. Consequently, this can lead to adrenal fatigue. This includes, inability to get up in the morning, handle stress, craving for salty food, overuse of stimulants such as coffee and a weak immune system.
-
Growth Hormone (GH)
Growth Hormone is secreted by the anterior pituitary gland. This hormone affects cellular activity and metabolism of protein, carbohydrates and fat.
Additionally, pain prompts the pituitary gland to increase secretion of GH. Excessive GH results in increased blood glucose level and insulin resistance.
However, a deficiency of GH can cause muscle weakness and fatigue. Therefore, GH is an important element in pain management.
-
Cytokines
Cytokines are produced locally by peripheral cells local to the injury and by cells in the dorsal horn of the spinal cord and brain.
Immediately after an injury, sensory nerve endings get sensitised and stimulate production of noxious mediators. Similarly, they stimulate production of pain neurotransmitters. Finally, there is increased production of receptors on the neurons to increase sensitivity.
Simultaneously, cell activity is reduced. So, the increased sensitivity results in amplification of pain, triggering the HPA axis and causing fever.
Blocking the activity of pro-inflammatory cytokines can reduce pain. Application of cold compress locally may reduce production of cytokines.
-
Prostaglandin
This hormone like substance participates in a wide range of body functions such as contraction and relaxation of muscles, dilation and constriction of blood vessels, blood pressure and modulation of inflammation. Generally, prostaglandins are not secreted by any gland, but manufactured at the site where tissue is damaged or infected. Here, they cause inflammation, fever and pain as a part of the healing process.
High levels of prostaglandins can cause pain, cramps, and muscle distress. So, this hormone needs to be controlled and managed.
-
Methadone
Methadone is a synthetic analgesic that causes sedation and relaxation. Additionally, methadone is also used in treating narcotic addiction. Slowly, it is being accepted as a drug for treating cancer pain.
However, it is possible to supplement methadone by making the dietary changes as given in the solution section below.
School of Yoga explains natural hormones which can help in managing pain
The quartet of happiness: Dopamine, serotonin, oxytocin and endorphins are responsible for our happiness and the best part is that we can control their secretion. So, increasing the production of these hormones in the body, it is possible to improve our ability to manage pain.

-
Oxytocin
Oxytocin is secreted by the hypothalamus. It is released when people bond socially or get physically intimate with each other. In fact, oxytocin plays a critical role in managing cardiac and kidney homeostasis. Also, oxytocin induces sleep and has a tranquilising and calming effect on us. Consequently, this counters the effect of steroids which are secreted as a side effect of pain.
-
Endorphins
Endorphins are chemicals produced naturally by the body to fight pain. They are released when we get hurt or in any stress situation, but also during exercise, laughter or sex. Additionally, endorphins, while reducing the sensation of pain, increase the feeling of euphoria. Also, these chemicals boost the immune system when activated.
In fact, endorphins are released after any aerobic exercise and last for up to 24 hours. Importantly, endorphins are also released by acupuncture, massage, hot bath etc.
-
Dopamine and Serotonin
Dopamine and Serotonin are neurotransmitters. Neurotransmitters are chemical messengers that transmit signals between to other nerve cells and regulate the countless functions performed by the body, from sleep to metabolism.
Dopamine helps control the brain’s reward and pleasure centers. Thus, dopamine drives motivation and helps regulate movement and emotional responses. Consequently, it is released during pleasure seeking situations such as food, sex etc. The pleasure we experience after successful conclusion of any activity is the rush of dopamine. Conversely, deficiency of dopamine in the brain can result in movements becoming delayed and uncoordinated. In fact, the loss of motivation, stress and trauma could be on account of low levels of dopamine.
Serotonin is also a neurotransmitter. It triggers moods such as anxiety in all areas, including OCD (obsessive compulsive disorder).
Other effects of Dopamine and Serotonin
The difference between dopamine and serotonin is that dopamine affects motivation while serotonin affects mood. Also, both dopamine and serotonin affect digestion. Dopamine affects the release of insulin from our pancreas and peristalsis. Additionally, dopamine has a protective effect on the mucosal layer in the gastrointestinal tract.
95% of our body’s serotonin is found in our gut. In fact, serotonin is released when food enters the small intestine where it helps in creating peristalsis. So, low serotonin can result in constipation.
Sleep – Sleep is controlled by the pineal gland which produces melatonin. Dopamine induces wakefulness and reduces production of melatonin. However, serotonin has a deeper impact. Firstly, induces the pineal gland to produce melatonin. Also, it affects wakefulness and prevents REM (rapid eye movement). Consequently, this affects management of pain.
So, dopamine and serotonin are two neurotransmitters which impact the management of pain by affecting the brain and gut. Consequently, an imbalance will affect mental health, digestion and sleep.
Importantly, seeds such as sunflower or pumpkin, nuts such as almonds and walnuts and herbs such as ginseng, fenugreek or peppermint increase dopamine levels.
-
GABA (gamma-aminobutyric acid)
GABA is a chemical in the brain which helps regulate nerve activity. So, it is found to be reduced in people with mood and anxiety issues.
Asana and pranayama such as kapalabhati can fire up the thalamus and increase levels of GABA. Also, magnesium, which iis found in bananas, increases GABA and reduces stress and anxiety.
Importantly, a diet which includes grains, leafy vegetables, dark chocolate etc can increase levels of GABA.
School of Yoga explains – Solutions to Pain

While it is obvious that chronic pain management requires lifestyle change, natural pain management cannot replace medical intervention.
Importantly, while natural remedies may not reduce pain, they will increase the body’s ability to manage pain. Also, natural remedies will increase the body’s resilience and increase the person’s stamina or reserves to overcome the ailment. Additionally, these remedies will help in purging the body of the toxins created by pain and pain management drugs.
School of Yoga explains pain management using diet
Before starting any of these remedies, it is recommended that the practitioner discusses the remedy with his or her physician.
- Include foods with low saturated fats such as cottage cheese, almonds, walnuts, dark chocolate etc. Good fats reduce the impact of Growth Hormone (GH).
- Increase intake of food rich in omega 3’s such as walnuts, flax and pumpkin seeds. This is good form managing cytokines.
- Reduce sugar and salt intake
- Eat foods rich in tyrosine (protein rich diet) which is a building block of dopamine. This includes, bananas, almonds, avocados, cottage cheese (paneer), curds/ yogurt, beans/ lentils, soy/ tofu, eggs, fish and chicken. Also, dark chocolate increases production of tyrosine and phenylaline.
- Go organic. This reduces the number of toxins that the organs need to process. Also, natural grains increase insulin levels which in turn result in production of serotonin.
- Increase vegetable/ nuts/ grains/ fruit content – vegetables and beans have all the required minerals and vitamins. Also, they increase fibre content – these are beans, dark greens such as spinach, broccoli, red cabbage, herbs such as ginger and fruits such as papaya, oranges and cantaloupe.
- Meat – avoid red meats. If you must eat meat, try to choose boiled, baked, broiled or steamed white meat and fish. While red meats offer an easy source of protein, they also have side effects such as increased bad cholesterol, lower fibre levels etc.
- Chocolate increases release of endorphins and reduces growth hormone.
School of Yoga explains pain management using exercise and other aspects

- Exercise – Cortisol control can be done by 20-30 minutes of regular exercise such as walking, biking etc. which leeches cortisol from the blood stream. Yoga, pranayama and meditation impact anxiety and naturally reduce generation of cortisol. Also, during exercise, the brain releases serotonin, endorphins and dopamine which help naturally control pain.
- Meditate for 15 minutes. Meditation reduces anxiety. So, this reduces the secretion of cortisol. Also, it increases the level of positivity, thus ensuring increased ability to manage pain.
- Laughter and group therapy reduces cortisol levels and increases releases of dopamine, oxytocin and endorphins. So, networking and talking to people helps manage pain.
- Sex increases the feeling of being wanted and increases levels of oxytocin and endorphins.
- Sleep – sleep allows the body to rebuild itself.
- Music – music has been found to reduce stress and increase the feeling of wellbeing.
- Massage – massage is an effective tool to increase blood circulation to the affected parts of the body. Also, they have a relaxing effect on the muscles, leading to reduction in cortisol levels.
School of Yoga explains Yoga Solutions to Pain
It is assumed that a person in chronic pain will be suffering from a debilitating illness. So, the ability to perform exercise may be limited.
Pain management may be divided into the following areas;
- Increased resistance to air and water infection by strengthening the adenoids, thyroid and the pharynx. Practice sundara-viparītakaraṇi and any form of prāṇāyāma. Also, if possible, and health permitting, practice sarvāngāsana, matsyāsana, bhramarī, ujjeyī and bhastrikā prāṇāyāma are useful.
- Increasing blood flow to the brain, especially the pituitary/ hypothalamus area. Sundara-viparītakaraṇi will help. If possible, the person may include śirasāsana, sarvāngāsana, matsyāsana, and ujjeyī prāṇāyāma.
- Breathing is a psychosomatic process which affects the stress levels in the body. Also, prāṇāyāma can counteract the reduction in oxygen levels in the blood due to adrenocorticotrophin (ACTH). Hence, it is important to ensure breathing is deep, regular and rhythmic to ensure that stress is reduced to bring back homeostasis. Nāḍī-śuddhi prāṇāyāma and meditation (dhyāna) must be practiced.
- It is important that the practitioner also keep a clean digestive system as it affects the breathing cycle. Pavanamuktāsana, śalabhāsana and dhanurāsana should be practiced if possible.
What is an ideal the āsana plan for pain management?
- Beginner – 3 months – all āsana to be performed slowly and after OK from doctor.
- Intermediate – 3 months – all āsana to be performed only after improvement is detected and after OK from doctor. Estimated time – 30 mins.
- Final – all āsana to be performed only after substantial improvement is detected and after OK from doctor. Estimated time – 45 mins.
| Āsana | Beginner | Intermediate | Final | |
| No | Time frame | 3 months | 3 months | thereafter |
| 1 | Padmāsana | 3 minutes | 3 minutes | 3 minutes |
| 2 | Sukhāsana | 3 minutes | 3 minutes | 3 minutes |
| 3 | Trikonāsana | 2 | 2 | 2 |
| 4 | Pādahastāsana | 2 | 2 | 2 |
| 5 | Tadāsana | 2 | 3 | 3 |
| 6 | Majriāsana | 2 | 2 | 3 |
| 7 | Makarāsana | 2 | 2 | 3 |
| 8 | Adho-mukha-śvānāsana | 2 | 3 | 3 |
| 9 | Sethubandhāsana | 2 | 3 | 3 |
| 10 | Arda-halāsana | 2 | 3 | 4 |
| 11 | Naukāsana | 1 | 2 | 3 |
| 12 | Sundara-viparītakaraṇi (essential) | 3 x 2 mts | 5 x 2 mts | 15 minutes |
| 13 | Sarvāngāsana (if possible) | 3 minutes | 5 minutes | 10 minutes |
| 14 | Matsyāsana (if possible) | – | – | 1 x 10 counts |
| 15 | Arda-matsyendrāsana | 1 x 10 counts | 2 x 10 counts | 2 x 10 counts |
| 16 | Nāḍī-śuddhi– prāṇāyāma (important) | 5 x 2 cycles | 5 x 2 cycles | 5 x 2 cycles |
| 17 | Śavāsana | 5 minutes | 5 minutes | 5 minutes |
| 18 | Meditation – dhyāna (sit in silence and focus on the breath – very important) | 10 minutes | 15 minutes | 20 minutes |